A human body producing its own medications on demand sounds like science fiction. Instead, researchers such as Northwestern Engineering’s Jonathan Rivnay are working today to make that technology a reality, and soon.
Rivnay and collaborators Paul E. Sheehan and Omid Veiseh wrote about this emerging treatment in the commentary article “Are Implantable, Living Pharmacies Within Reach?” published October 17 in the journal Science.
“Imagine combining synthetic biology (engineering a cell’s DNA to create new functions or modify existing ones) with bioelectronics (electrical control over physiological function) in ways that facilitate sensing, actuation, and wireless communication to regulate the production of a drug inside a patient,” the team wrote. “This biohybrid concept could be revolutionary, substantially reducing manufacturing costs and consequently improving patient access and adherence to treatments and, ultimately, health outcomes.”

Jonathan Rivnay
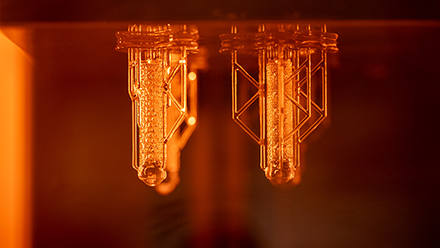
Rivnay is a professor of biomedical engineering and of materials science and engineering at the McCormick School of Engineering. His research group engineers organic (polymeric) and biohybrid bioelectronic materials, devices, and systems for interfacing between the complex world of biology and traditional optoelectronics. Over the past five years, Rivnay and collaborators have been working on these concepts, with funding from the Defense Advanced Research Projects Agency, ARPA-H, and the Juvenile Diabetes Research Foundation.
Sheehan is program manager, resilient systems at ARPA-H; and Veiseh is a professor of bioengineering at Rice University.
Below are three key takeaways from the team’s paper.
Biologic drugs are helpful, but can be improved upon
Biologic drugs – treatments sourced from living organisms – have been beneficial to patients since the turn of the century. According to the commentary, around 330 biologic drugs have been approved by the US Food and Drug Administration, including treatments for autoimmune diseases, cancer, and many others. The drugs’ global market size is estimated to be $510 million and projected to jump to $1.3 trillion by 2033.
That does not mean, however, that these drugs are perfected.
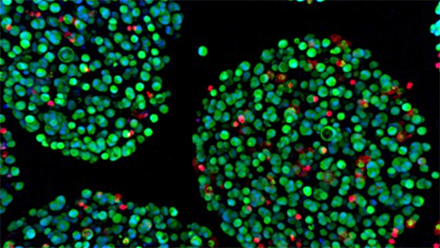
Biologic drug treatments are expensive because of production costs, including stabilization, purification, packaging, and marketing. Their efficacy also declines as a patient’s immune system reacts to modified biologics or changes with illness, raising the long-term costs for a patient as diseases need management. Cell-based therapeutics have been developed to address many of these concerns, where engineered cells serve a drug-producing factories in the body. Such approaches would delivery continuous therapies so long as cells were viable in the body. Although some treatments can be implemented continuously without dosing control, many therapies do require regulation.
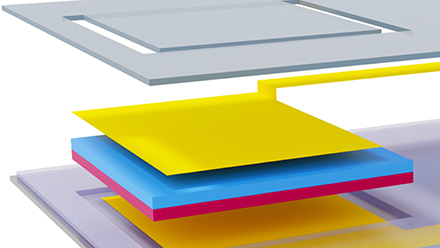
Bioelectronics could be a solution, Rivnay and his colleagues wrote, because they could flexibly implement control algorithms for either actuation or simulation. Miniaturized electronics have been adapted for wearable and implantable settings to work with the heart, ears, and even the brain. Current systems even implement electronic control of drug pumps using commercial continuous glucose monitors to manage Type I diabetes.
However, the ability to have real-time glycemic control for diabetes patients – without devices attached to their bodies – would be groundbreaking.
“The next frontier in biohybrid systems is to refine and better integrate cell and electronic systems so that production of a biologic in vivo can last long term and can occur on demand,” the authors wrote. “Here, a central goal is developing gene circuits that turn on or off drug synthesis when the engineered cells are activated by an electrical, optical, or even mechanical stimulus.”